Non-human primates in pre-clinical research
Two main species of non-human primates are used in the pre-clinical research setting: Cynomolgus (Macaca fascicularis) and Rhesus (Macaca mulatta) macaques. During the development of novel therapeutics for human diseases and infections, the majority of early research and development is performed in small animal models, such as rodents. However, inherent differences exist between rodent and human organs, tissues, and cellular components. Thus, to increase translatability of new therapeutics, the use of macaques is becoming a critical pre-clinical step and is useful for evaluating the dose requirements and toxicologic effects of biotherapeutics and pharmaceuticals. Due to their genetic and physiologic similarities with humans, macaques comprise a unique and highly relevant model organism for evaluating the safety, efficacy, pharmacokinetics, and pharmacodynamics of novel therapeutics.
Table 1: Recent examples of research contributions of NHP to human health
1980s
-
First animal model for research on Parkinson’s disease
-
First Hepatitis B vaccine
-
Rhesus monkey model for AIDS used to establish the effectiveness of AZT
1990s
-
Primate embryonic stem cells studies for understanding on reproduction and genetic disorders
-
Monkey model developed for diabetes research
-
Rhesus & Cynomolgus monkey kidneys developed for use in diagnosing influenza
-
Development of anthrax vaccine
-
Development of treatments for systemic lupus erythematosus (SLE)
2000s
-
Monkey model developed for studying the effects of malaria in pregnant women and their offspring
-
Rhesus monkeys are prime model for HIV treatments and vaccines development
-
Food-borne pathogen, Cyclospora, characterized in primates
-
Contributed to the advance of Human pluripotent stem cell discoveries
-
Effect of BPA on prenatal development
(Original source: National Primate Research Centers)
Toll-like Receptors and Type I Interferon
The ligation of host Toll-like receptors (TLRs) by bacterial and viral components results in production of type I interferons (IFNs) by many cell types, including plasmacytoid dendritic cells and macrophages. Type I IFNs (IFN-Alpha and -Beta) play pivotal roles in both protective and pathologic immunity. Clinically, maintenance of serum type I IFN levels within a range that is advantageous for limiting viral infections, while simultaneously avoiding the onset of autoimmunity, is crucial. Recently there has been a flurry of attempts to design next-level adjuvants that take advantage of nucleotide-sensing pathways to induce type I IFN and produce an enhanced immune response. In addition, for autoimmune diseases such as rheumatoid arthritis (RA), antagonists to TLRs 7 and 9 have been developed as novel therapeutics to dampen excessive IFN production. In contrast, TLR 7 and 9 agonists have been evaluated for their ability to induce IFN-Alpha and enhance protective immunity against Hepatitis C viral infections. Both of these strategies necessitate careful monitoring of IFN-Alpha levels to protect against the development of an immunocompromised state or other detrimental side effects. Therefore, use of pre-clinical macaque models affords the unique opportunity to test novel therapeutics for efficacy, potency, safety, toxicology, and off-target side effects prior to beginning Phase I trials in humans.
Receptor
Typical Ligands
TLR-1
Bacterial lipoproteins
TLR-2
Lipoteichoic acid (LTA), peptidoglycan (PGN), Bacterial lipoproteins, zymosan
TLR-3
Double-strand RNA
TLR-4
Lipopolysaccharide (LPS), RSVF protein, Viral envelope protein MMTV
TLR-5
Flagellin
TLR-6
LTA, Diacyl lipoproteins, zymosan
TLR-7
ssRNA, imidazoquinolines
TLR-8
ssRNA, imidazoquinolines
TLR-9
Unmethylated CpG DNA
TLR-11
Uropathogenic bacterial, profilin-like protein
Therapeutics Targeting Type I IFNs and TLR Pathways
Some of the most exciting new drugs currently in development are small molecule agonists and antagonists of TLRs (Toll-Like Receptors). TLRs are highly conserved receptors of the innate immune system that recognize pathogen-associated molecular patterns (PAMPs). These short recognition sequences are found in bacterial and viral components ranging from bacterial lipopolysaccharide (LPS) and flagellin to double stranded RNA and unmethylated CpG DNA motifs. Ligation of the TLR receptors that bind dsRNA, LPS, ssRNA, or CpG DNA (TLRs 3, 4, 7, 8, and 9, respectively) initiates signaling cascades that culminate in the production of type I IFNs, such as IFN-Alpha and -Beta, as well as proinflammatory cytokines and chemokines3,4 (Figure 1). Current studies are focused on the use of TLR antagonists for treatment of SLE and asthma5,6. Additionally, TLR agonists are readily being applied as adjuvants in a number of vaccine trials7. These include vaccines against viral diseases ranging from seasonal influenza8 to HIV9, as well as for use in cancer vaccines10. Many TLR agonists and antagonists have progressed to clinical trial testing for safety and efficacy (www.clinicaltrials.gov).
Because IFN-Alpha production is a major downstream readout indicative of TLR activation, it is frequently utilized in the research setting and in clinical trials as an indicator of TLR agonist potency in vitro (tissue culture media) and in vivo (serum or plasma). This is particularly true for studies on novel TLR-based therapies that employ or inhibit IFN-Alpha production as an intended component of their mechanisms of action. Of particular relevance are several preclinical studies and clinical trials involving novel therapeutic TLR7 agonists that induce IFN-Alpha to protect against Hepatitis C infections and TLR 7/8 antagonists that reduce IFN-Alpha levels for the treatment of rheumatoid arthritis6, 7. In addition, an inhaled TLR7 agonist has been tested in NHPs and an inhaled TLR9 agonist has been found to be well tolerated in humans for treatment of allergic diseases including asthma. For formulations such as these that are designed for localized application, it is of central importance that serum biomarkers, including type I IFNs, be quantitated to assess any off-target, systemic inflammatory responses5,6.
Type I IFN and HIV/SIV
The relationship between IFN and HIV-1 infection is complex. Type I IFNs have been shown to inhibit replication of HIV-1 in cell culture and treatment of HIV-1 infected patients with type I IFN produces a marked, but transient, decrease in plasma viral load. However, in NHP models of SIV infection, which closely mimics HIV infection in humans, and during chronic HIV infection of humans, production of IFN and its downstream effects correlate with disease progression11. The reason for this remains unclear, and future study is warranted in order to aid in development of therapeutics. Acute production of IFN-Alpha following SIV infection of NHPs has been shown to be mediated by plasmacytoid dendritic cells (pDCs). It has been shown in other model systems that during the acute to chronic disease transition period, IFN-Alpha levels return to baseline. This shift in IFN production is believed to be due to activation-induced exhaustion of pDCs and subsequent increase in pre-DC precursors, which lack the ability to produce type I IFN12.
NHP models of other viruses
Arguably, the most frequently utilized application of NHP models is for virology and vaccine studies. This is due to the ability of many human viruses to infect NHPs without the need for adaptation, and to the similarities in the immune response to viral infection. Viruses that have undergone testing in NHPs include Dengue, Ebola, Marburg, and West Nile18–20. It especially makes sense to use NHPs to study viruses that cause high fatality rates in humans, as vaccine efficacy cannot readily be tested without this model.
Summary
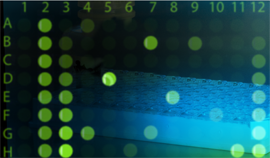
IFNs play a pivotal role not only in protective responses to many infections and diseases, but also in the generation of side effects and pathological sequelae when its production is unchecked. The ability to precisely quantify this family of cytokines in NHP is valuable not only in basic research but also for vaccine development and drug discovery. Accurate measurement of nonhuman primate IFN alpha and IFN-Beta in serum, plasma, and cell culture media by robust immunoassays such as PBL’s Cynomolgus IFN-Alpha and Cynomolgus IFN-Beta ELISAs would certainly enable NHP-based discoveries advance further.
References:
1. Brooks DG, Ha SJ, Elsaesser H, Sharpe AH, Freeman GJ, Oldstone MBA. IL-10 and PD-L1 operate through distinct pathways to suppress T-cell activity during persistent viral infection. Proc Natl Acad Sci U S A. 2008. doi:10.1073/pnas.0811139106
2. Ng CT, Sullivan BM, Teijaro JR, et al. Blockade of interferon beta, but not interferon alpha, signaling controls persistent viral infection. Cell Host Microbe. 2015. doi:10.1016/j.chom.2015.04.005
3. Petzke MM, Brooks A, Krupna MA, Mordue D, Schwartz I. Recognition of Borrelia burgdorferi , the Lyme Disease Spirochete, by TLR7 and TLR9 Induces a Type I IFN Response by Human Immune Cells . J Immunol. 2009. doi:10.4049/jimmunol.0901390
4. Noppert SJ, Fitzgerald KA, Hertzog PJ. The role of type I interferons in TLR responses. Immunol Cell Biol. 2007. doi:10.1038/sj.icb.7100099
5. Bell J, Dymond M, Biffen M, et al. Temporal cytokine and lymphoid responses to an inhaled TLR7 antedrug agonist in the cynomolgus monkey demonstrates potential safety and tolerability of this approach. Toxicol Appl Pharmacol. 2018. doi:10.1016/j.taap.2017.11.002
6. Jackson S, Candia AF, Delaney S, et al. First-in-Human Study With the Inhaled TLR9 Oligonucleotide Agonist AZD1419 Results in Interferon Responses in the Lung, and Is Safe and Well-Tolerated. Clin Pharmacol Ther. 2018. doi:10.1002/cpt.938
7. Steinhagen F, Kinjo T, Bode C, Klinman DM. TLR-based immune adjuvants. Vaccine. 2011. doi:10.1016/j.vaccine.2010.08.002
8. Rudicell RS, Garinot M, Kanekiyo M, et al. Comparison of adjuvants to optimize influenza neutralizing antibody responses. Vaccine. 2019. doi:10.1016/j.vaccine.2019.08.030
9. Francica JR, Zak DE, Linde C, et al. Innate transcriptional effects by adjuvants on the magnitude, quality, and durability of HIV envelope responses in NHPs. Blood Adv. 2017. doi:10.1182/bloodadvances.2017011411
10. Li JK, Balic JJ, Yu L, Jenkins B. TLR agonists as adjuvants for cancer vaccines. In: Advances in Experimental Medicine and Biology. ; 2017. doi:10.1007/978-981-10-5987-2_9
11. Doyle T, Goujon C, Malim MH. HIV-1 and interferons: Who’s interfering with whom? Nat Rev Microbiol. 2015. doi:10.1038/nrmicro3449
12. Macal M, Jo Y, Dallari S, et al. Self-Renewal and Toll-like Receptor Signaling Sustain Exhausted Plasmacytoid Dendritic Cells during Chronic Viral Infection. Immunity. 2018. doi:10.1016/j.immuni.2018.03.020
13. Katze MG, He Y, Gale M. Viruses and interferon: A fight for supremacy. Nat Rev Immunol. 2002. doi:10.1038/nri888
14. Brok J, Gluud LL, Gluud C. Ribavirin plus interferon versus interferon for chronic hepatitis C. Cochrane Database Syst Rev. 2005.
15. Li L, Han DK, Lu J. Interferon-Alpha induced severe thrombocytopenia: A case report and review of the literature. World J Gastroenterol. 2010. doi:10.3748/wjg.v16.i11.1414
16. Dhillon S, Kaker A, Dosanjh A, Japra D, Vanthiel DH. Irreversible pulmonary hypertension associated with the use of interferon alpha for chronic hepatitis C. Dig Dis Sci. 2010. doi:10.1007/s10620-010-1220-7
17. Ottosen S, Parsley TB, Yang L, et al. In Vitro antiviral activity and preclinical and clinical resistance profile of miravirsen, a novel anti-hepatitis C virus therapeutic targeting the human factor miR-122. Antimicrob Agents Chemother. 2015. doi:10.1128/AAC.04220-14
18. Estes JD, Wong SW, Brenchley JM. Nonhuman primate models of human viral infections. Nat Rev Immunol. 2018. doi:10.1038/s41577-018-0005-7
19. Warren TK, Wells J, Panchal RG, et al. Protection against filovirus diseases by a novel broad-spectrum nucleoside analogue BCX4430. Nature. 2014. doi:10.1038/nature13027
20. Widman DG, Ishikawa T, Giavedoni LD, et al. Evaluation of RepliVAX WN, a single-cycle flavivirus vaccine, in a non-human primate model of west nile virus infection. Am J Trop Med Hyg. 2010. doi:10.4269/ajtmh.2010.09-0310
Non-human primates in pre-clinical research
Two main species of non-human primates are used in the pre-clinical research setting: Cynomolgus (Macaca fascicularis) and Rhesus (Macaca mulatta) macaques. During the development of novel therapeutics for human diseases and infections, the majority of early research and development is performed in small animal models, such as rodents. However, inherent differences exist between rodent and human organs, tissues, and cellular components. Thus, to increase translatability of new therapeutics, the use of macaques is becoming a critical pre-clinical step and is useful for evaluating the dose requirements and toxicologic effects of biotherapeutics and pharmaceuticals. Due to their genetic and physiologic similarities with humans, macaques comprise a unique and highly relevant model organism for evaluating the safety, efficacy, pharmacokinetics, and pharmacodynamics of novel therapeutics.
Table 1: Recent examples of research contributions of NHP to human health
|
1980s |
|
|
1990s |
|
|
2000s |
|
(Original source: National Primate Research Centers)
Toll-like Receptors and Type I Interferon
The ligation of host Toll-like receptors (TLRs) by bacterial and viral components results in production of type I interferons (IFNs) by many cell types, including plasmacytoid dendritic cells and macrophages. Type I IFNs (IFN-Alpha and -Beta) play pivotal roles in both protective and pathologic immunity. Clinically, maintenance of serum type I IFN levels within a range that is advantageous for limiting viral infections, while simultaneously avoiding the onset of autoimmunity, is crucial. Recently there has been a flurry of attempts to design next-level adjuvants that take advantage of nucleotide-sensing pathways to induce type I IFN and produce an enhanced immune response. In addition, for autoimmune diseases such as rheumatoid arthritis (RA), antagonists to TLRs 7 and 9 have been developed as novel therapeutics to dampen excessive IFN production. In contrast, TLR 7 and 9 agonists have been evaluated for their ability to induce IFN-Alpha and enhance protective immunity against Hepatitis C viral infections. Both of these strategies necessitate careful monitoring of IFN-Alpha levels to protect against the development of an immunocompromised state or other detrimental side effects. Therefore, use of pre-clinical macaque models affords the unique opportunity to test novel therapeutics for efficacy, potency, safety, toxicology, and off-target side effects prior to beginning Phase I trials in humans.
|
Receptor |
Typical Ligands |
|
TLR-1 |
Bacterial lipoproteins |
|
TLR-2 |
Lipoteichoic acid (LTA), peptidoglycan (PGN), Bacterial lipoproteins, zymosan |
|
TLR-3 |
Double-strand RNA |
|
TLR-4 |
Lipopolysaccharide (LPS), RSVF protein, Viral envelope protein MMTV |
|
TLR-5 |
Flagellin |
|
TLR-6 |
LTA, Diacyl lipoproteins, zymosan |
|
TLR-7 |
ssRNA, imidazoquinolines |
|
TLR-8 |
ssRNA, imidazoquinolines |
|
TLR-9 |
Unmethylated CpG DNA |
|
TLR-11 |
Uropathogenic bacterial, profilin-like protein |
Therapeutics Targeting Type I IFNs and TLR Pathways
Some of the most exciting new drugs currently in development are small molecule agonists and antagonists of TLRs (Toll-Like Receptors). TLRs are highly conserved receptors of the innate immune system that recognize pathogen-associated molecular patterns (PAMPs). These short recognition sequences are found in bacterial and viral components ranging from bacterial lipopolysaccharide (LPS) and flagellin to double stranded RNA and unmethylated CpG DNA motifs. Ligation of the TLR receptors that bind dsRNA, LPS, ssRNA, or CpG DNA (TLRs 3, 4, 7, 8, and 9, respectively) initiates signaling cascades that culminate in the production of type I IFNs, such as IFN-Alpha and -Beta, as well as proinflammatory cytokines and chemokines3,4 (Figure 1). Current studies are focused on the use of TLR antagonists for treatment of SLE and asthma5,6. Additionally, TLR agonists are readily being applied as adjuvants in a number of vaccine trials7. These include vaccines against viral diseases ranging from seasonal influenza8 to HIV9, as well as for use in cancer vaccines10. Many TLR agonists and antagonists have progressed to clinical trial testing for safety and efficacy (www.clinicaltrials.gov).
Because IFN-Alpha production is a major downstream readout indicative of TLR activation, it is frequently utilized in the research setting and in clinical trials as an indicator of TLR agonist potency in vitro (tissue culture media) and in vivo (serum or plasma). This is particularly true for studies on novel TLR-based therapies that employ or inhibit IFN-Alpha production as an intended component of their mechanisms of action. Of particular relevance are several preclinical studies and clinical trials involving novel therapeutic TLR7 agonists that induce IFN-Alpha to protect against Hepatitis C infections and TLR 7/8 antagonists that reduce IFN-Alpha levels for the treatment of rheumatoid arthritis6, 7. In addition, an inhaled TLR7 agonist has been tested in NHPs and an inhaled TLR9 agonist has been found to be well tolerated in humans for treatment of allergic diseases including asthma. For formulations such as these that are designed for localized application, it is of central importance that serum biomarkers, including type I IFNs, be quantitated to assess any off-target, systemic inflammatory responses5,6.
Type I IFN and HIV/SIV
The relationship between IFN and HIV-1 infection is complex. Type I IFNs have been shown to inhibit replication of HIV-1 in cell culture and treatment of HIV-1 infected patients with type I IFN produces a marked, but transient, decrease in plasma viral load. However, in NHP models of SIV infection, which closely mimics HIV infection in humans, and during chronic HIV infection of humans, production of IFN and its downstream effects correlate with disease progression11. The reason for this remains unclear, and future study is warranted in order to aid in development of therapeutics. Acute production of IFN-Alpha following SIV infection of NHPs has been shown to be mediated by plasmacytoid dendritic cells (pDCs). It has been shown in other model systems that during the acute to chronic disease transition period, IFN-Alpha levels return to baseline. This shift in IFN production is believed to be due to activation-induced exhaustion of pDCs and subsequent increase in pre-DC precursors, which lack the ability to produce type I IFN12.
NHP models of other viruses
Arguably, the most frequently utilized application of NHP models is for virology and vaccine studies. This is due to the ability of many human viruses to infect NHPs without the need for adaptation, and to the similarities in the immune response to viral infection. Viruses that have undergone testing in NHPs include Dengue, Ebola, Marburg, and West Nile18–20. It especially makes sense to use NHPs to study viruses that cause high fatality rates in humans, as vaccine efficacy cannot readily be tested without this model.
Summary
IFNs play a pivotal role not only in protective responses to many infections and diseases, but also in the generation of side effects and pathological sequelae when its production is unchecked. The ability to precisely quantify this family of cytokines in NHP is valuable not only in basic research but also for vaccine development and drug discovery. Accurate measurement of nonhuman primate IFN alpha and IFN-Beta in serum, plasma, and cell culture media by robust immunoassays such as PBL’s Cynomolgus IFN-Alpha and Cynomolgus IFN-Beta ELISAs would certainly enable NHP-based discoveries advance further.
References:
1. Brooks DG, Ha SJ, Elsaesser H, Sharpe AH, Freeman GJ, Oldstone MBA. IL-10 and PD-L1 operate through distinct pathways to suppress T-cell activity during persistent viral infection. Proc Natl Acad Sci U S A. 2008. doi:10.1073/pnas.0811139106
2. Ng CT, Sullivan BM, Teijaro JR, et al. Blockade of interferon beta, but not interferon alpha, signaling controls persistent viral infection. Cell Host Microbe. 2015. doi:10.1016/j.chom.2015.04.005
3. Petzke MM, Brooks A, Krupna MA, Mordue D, Schwartz I. Recognition of Borrelia burgdorferi , the Lyme Disease Spirochete, by TLR7 and TLR9 Induces a Type I IFN Response by Human Immune Cells . J Immunol. 2009. doi:10.4049/jimmunol.0901390
4. Noppert SJ, Fitzgerald KA, Hertzog PJ. The role of type I interferons in TLR responses. Immunol Cell Biol. 2007. doi:10.1038/sj.icb.7100099
5. Bell J, Dymond M, Biffen M, et al. Temporal cytokine and lymphoid responses to an inhaled TLR7 antedrug agonist in the cynomolgus monkey demonstrates potential safety and tolerability of this approach. Toxicol Appl Pharmacol. 2018. doi:10.1016/j.taap.2017.11.002
6. Jackson S, Candia AF, Delaney S, et al. First-in-Human Study With the Inhaled TLR9 Oligonucleotide Agonist AZD1419 Results in Interferon Responses in the Lung, and Is Safe and Well-Tolerated. Clin Pharmacol Ther. 2018. doi:10.1002/cpt.938
7. Steinhagen F, Kinjo T, Bode C, Klinman DM. TLR-based immune adjuvants. Vaccine. 2011. doi:10.1016/j.vaccine.2010.08.002
8. Rudicell RS, Garinot M, Kanekiyo M, et al. Comparison of adjuvants to optimize influenza neutralizing antibody responses. Vaccine. 2019. doi:10.1016/j.vaccine.2019.08.030
9. Francica JR, Zak DE, Linde C, et al. Innate transcriptional effects by adjuvants on the magnitude, quality, and durability of HIV envelope responses in NHPs. Blood Adv. 2017. doi:10.1182/bloodadvances.2017011411
10. Li JK, Balic JJ, Yu L, Jenkins B. TLR agonists as adjuvants for cancer vaccines. In: Advances in Experimental Medicine and Biology. ; 2017. doi:10.1007/978-981-10-5987-2_9
11. Doyle T, Goujon C, Malim MH. HIV-1 and interferons: Who’s interfering with whom? Nat Rev Microbiol. 2015. doi:10.1038/nrmicro3449
12. Macal M, Jo Y, Dallari S, et al. Self-Renewal and Toll-like Receptor Signaling Sustain Exhausted Plasmacytoid Dendritic Cells during Chronic Viral Infection. Immunity. 2018. doi:10.1016/j.immuni.2018.03.020
13. Katze MG, He Y, Gale M. Viruses and interferon: A fight for supremacy. Nat Rev Immunol. 2002. doi:10.1038/nri888
14. Brok J, Gluud LL, Gluud C. Ribavirin plus interferon versus interferon for chronic hepatitis C. Cochrane Database Syst Rev. 2005.
15. Li L, Han DK, Lu J. Interferon-Alpha induced severe thrombocytopenia: A case report and review of the literature. World J Gastroenterol. 2010. doi:10.3748/wjg.v16.i11.1414
16. Dhillon S, Kaker A, Dosanjh A, Japra D, Vanthiel DH. Irreversible pulmonary hypertension associated with the use of interferon alpha for chronic hepatitis C. Dig Dis Sci. 2010. doi:10.1007/s10620-010-1220-7
17. Ottosen S, Parsley TB, Yang L, et al. In Vitro antiviral activity and preclinical and clinical resistance profile of miravirsen, a novel anti-hepatitis C virus therapeutic targeting the human factor miR-122. Antimicrob Agents Chemother. 2015. doi:10.1128/AAC.04220-14
18. Estes JD, Wong SW, Brenchley JM. Nonhuman primate models of human viral infections. Nat Rev Immunol. 2018. doi:10.1038/s41577-018-0005-7
19. Warren TK, Wells J, Panchal RG, et al. Protection against filovirus diseases by a novel broad-spectrum nucleoside analogue BCX4430. Nature. 2014. doi:10.1038/nature13027
20. Widman DG, Ishikawa T, Giavedoni LD, et al. Evaluation of RepliVAX WN, a single-cycle flavivirus vaccine, in a non-human primate model of west nile virus infection. Am J Trop Med Hyg. 2010. doi:10.4269/ajtmh.2010.09-0310